With even the most minor impacts, a brain injury can occur changing everything about us in a split second. This affects the way a person thinks, acts, and feels. About 1.7 million cases of traumatic brain injury (“TBI”) occur in the U.S. every year costing an estimated $48-56 billion. The vast majority of TBI stem from car accidents followed by sport and recreational activities.

Sometimes called the invisible injury, it spares no expense for its wake of devastation and prolonged aftereffects. Symptoms can range from mild, moderate, or severe, depending on the nature and extent of damage to the brain. All, however, are serious. There are a variety of physical, emotional, and cognitive symptoms that someone can experience including:
Some brain injuries are obvious because they are visible. For example, a bullet wound through someone’s skull would be certainly obvious that a brain injury was suffered. Other times, there are mass lesion identified on an imaging study that can show blood clots (hematomas) and bruising (contusions) on the brain. Most brain injuries, however, are microscopic and can only be diagnosed through clinical assessment and diagnostic imaging using a variety of tools.
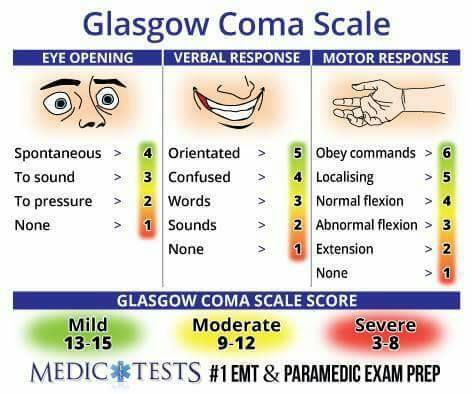
Victims with TBI need to undergo a systematic yet rapid evaluation in the emergency room. A neurological examination is normally performed utilizing the Glasgow Coma Scale (GCS). The Glasgow Coma Scale provides a practical method for assessment of impairment of conscious level in response to defined stimuli composed of 3 domains which are assessed separately and given numerical scores.
In addition to the GCS and physical examination, radiological studies of a patient can provide a more microanalysis of brain injuries. These diagnostic images show injuries that are not plainly visible to the naked eye.
Even without loss of consciousness or positive findings on an imaging study, there still can be a traumatic brain injury found through clinical correlation and assessment.
A clinical neuropsychology is a specialist dedicated to understanding the relationships between brain and behavior, particularly as these relationships can be applied to the diagnosis of brain disorder, assessment of cognitive and behavioral functioning, and the design of effective treatment. The neuropsychological can conduct a clinical interview with standardized diagnostic testing that focuses on a wide range of cognitive functions including attention, memory, language, academic skills, reasoning and problem solving, visuospatial ability, and sensory-motor skills. The neuropsychologist may also administer tests and questionnaires concerning psychological aspects of mood, emotional style, behavior, and personality. The results of this analysis interprets the relationship of a trauma-causing incident with the ongoing deficits caused by the accident.
There is no medication that can be given to cure a brain injury or prevent it from getting worse as the victim ages. Once a patient leaves the hospital, some may benefit from a rehabilitation program focused on physical, cognitive, and emotional deficits resulting from the trauma. These intensive programs can be expensive and prolonged with emphasis on compensatory strategies to help patients learn about their deficits and try to reach the maximum level of function allowed by their impairments through education and retraining.